Quality Outcomes & Tracking
MIPS & CLINICAL MANAGEMENT TOOLS
MediMobile uses our technology better. We offer quality initiative support and clinical management tools that focus on improving clinical quality outcomes for your patients.
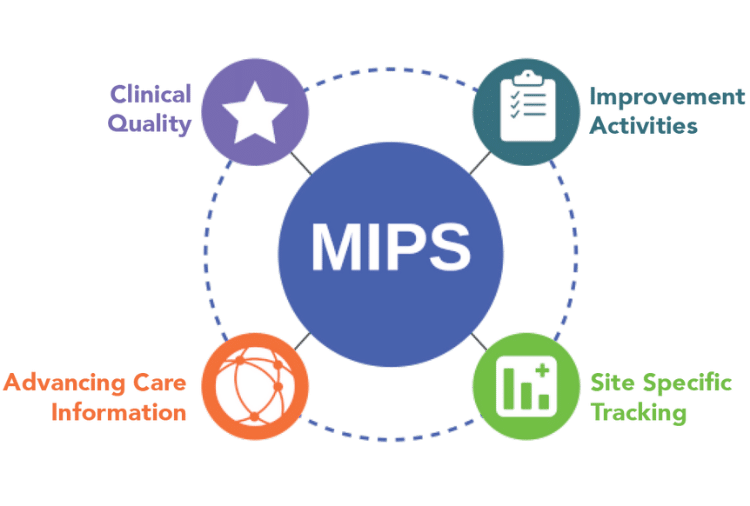
Our software rules engine can be tailored for selected MIPS measure capture, site specific quality measure customization and your organizational performance tracking.
-
Consulting and MIPS submission available
-
MediMobile rules engine can be tailored for selected MIPS measure capture
-
Providers capture data in real-time, ensuring no missing data per QPP processes
-
Facility specific quality measure customization and your organizational performance tracking
-
Organizational tracking of data such as discharge disposition or other quality tracking initiatives
-
Registry and claims submission options
-
Analytics and auditing
.png)